PUNCH Documentary Gives Insight Into The Tortuous Journeys Of Newborns To The Earth Through Traditional Birth Centres
According to UNICEF, in Nigeria, each year, about 262,000 babies die at birth, the which is the world’s second highest national total, while every day in Nigeria, 257 babies die within their first month of life.
Most of these children died from preventable causes such as premature birth, complications during delivery, and infections like sepsis and pneumonia, a violation of their basic right to survival.
Eniola Akinkuotu, PUNCH correspondent who visited several traditional birth centres, narrates the conditions in which a majority of pregnant women in rural communities give birth
One-month old Patience Okon may never remember the events of November 14, 2020 because she is too little to understand what happened. However, the scars on her face, hands, legs and other parts of her body will serve as a reminder of the suffering she faced on the day she was born.
Her unemployed mother had fallen into labour on the fateful day while her father, Daniel, who is a mechanic’s apprentice, took her to a traditional birth centre in Calabar, the Cross River State capital. Daniel said,
“On getting there, the attendant was very courteous. I left my wife at the centre and returned home to get a few things and also attend to my two other children.
“Moments later, I received a phone call that my wife had given birth. On returning to the centre, I saw the baby had been burnt. When I asked what happened, I was told that immediately the baby was born, a lantern which was used to light up the centre, fell on its side, spilled its kerosene, caught fire and burnt the baby.”
According to Daniel, the injured baby was taken to seven hospitals but the family was informed that there was little that could be done. Besides, the family was too poor to afford quality health services. They waited helplessly for help and luckily it arrived.
A viral social media post by a radio presenter, Uyoatta Esu aka Beezy Mouth, attracted donations from well-meaning Nigerians thereby giving baby Patience a chance to live. She will, however, need a series of plastic surgeries to be able to live a normal life.
While Patience has been given a second chance, the same cannot be said of the many babies born outside of health facilities who die moments after birth or during delivery. A visit by PUNCH correspondent to three traditional birth centres in different slums exposed the conditions in which poor and mostly illiterate women give birth.
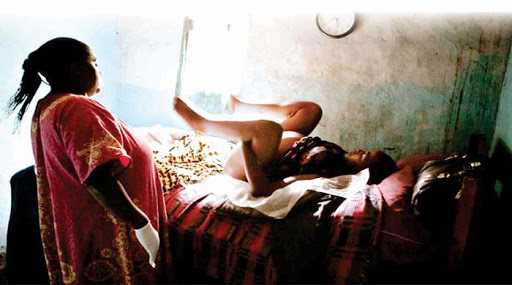
While some women are made to give birth on floors covered in linoleum next to candles in poorly lit rooms, others are forced to deliver their babies on torn mattresses with the aid of rechargeable lamps or telephone torches while deliveries are usually taken by unskilled birth attendants who pay little attention to hygiene in rooms that have torn mosquito nets.
There are no machines for monitoring blood pressure, no masks or proper spacing as recommended by the government due to the COVID-19 pandemic or ambulance services.
Findings by this newspaper showed that the poor attitude of health workers, the cost of delivery as well as the long distance of health facilities from rural areas made traditional birth centres attractive to poor and often uneducated women.
The reporter, who visited Halleluyah House, a traditional birth centre located in Aliwo, a slum in Ibadan North Local Government Area of Oyo State, perceived the stench oozing from the pit latrine which pregnant women and new mothers are forced to use.
At the centre, which is now being renovated by Help Mum Foundation, a Non-Governmental Organisation, the attendant, Omowunmi Olalere, said that she had taken delivery of hundreds of babies
Olalere said she could not attend any higher institution of learning because she did not pass the West African Senior School Certificate Examinations. She, however, said she trained as an auxiliary nurse in 1994.
The birth attendant explained that she initially did not want to open a centre but then pregnant women in the neighbourhood started reaching out to her for help and then she began taking deliveries with her bare hands on the floor for free.
“I took the delivery of twins in someone’s backyard. The mother could hardly walk to the hospital and I took their delivery on the bare floor. The twins are even abroad now,”
Olalere boasts.
She adds,
“I opened this centre about 10 years ago and I started using my two rooms. I then made two pit toilets in the compound but the stench almost killed the neighbourhood so I shut it because I didn’t have the money.”
The birth attendant admitted that she had no equipment or tools for taking deliveries and had to depend on NGOs for assistance.
She said she had a very high success rate at the centre because she had been called by God to do the job. The attendant, however, said complex cases were usually referred to hospitals, adding that hospitals had become a last resort because of the attitude of skilled health workers. Olalere adds,
“We are the ones that get the gloves, pads etc. Some come with plain material to use as pads that they will use as diapers. We are the ones that use our money to buy these things because we want to save life.
“We even prepare pap for pregnant women. But can hospitals do this? It is all about having human feelings. Some of these women have no husbands to support them or they are poor. How many people can health centres assist? Can a health worker use his personal money to buy pads for a woman?”
When asked to narrate the conditions in which pregnant women deliver babies at the centre, Olalere responded,
“Sometimes I get fed up. I take delivery of children with linoleum spread on the floor. When there is no light, we use candles. It is just recently that we started enjoying delivery of births due to the assistance of NGOs. I charge about N3,000 but if the person has no money, I will still help.”
At the centre was a 23-year-old woman, Taiwo Adeoye, who recently gave birth to a stillborn baby.
She, however, stated that she would not blame Hallelujah House for her loss because she believed the baby may have died even before she arrived at the centre. The unemployed woman also admitted that she could not afford ante-natal care and therefore could not do an ultrasound scan to monitor the progress of the foetus. Adeoye said,
“This was my first born but he died. I was about seven months pregnant. I started feeling uneasy and I was brought to this centre. On giving birth, I noticed that the baby neither opened his eyes nor cried. It was then that I was informed that the baby was dead.
“I was told that I probably wasn’t taking the proper medication during the pregnancy. In fact, a few days before I gave birth, I noticed that the baby wasn’t moving. Unfortunately, I didn’t have the money to do a scan.
“I was six months gone when I registered for ante-natal care at a government hospital. I took some injections at the hospital but I wasn’t going regularly because I didn’t have money. Usually, they collect N300 or N500 from me anytime I go to the hospital and I didn’t have the money.”
When asked if she would return to Hallelujah House to give birth when next she is pregnant, Adeoye responded, “As long as I don’t have the money, I will return here to give birth.”
At another centre in Omikunle slum known as Ayomide Faith Home, the birth attendant, Mrs. Alabi Testimony, says she started taking delivery of babies 11 years ago after training as an auxiliary nurse.
She explains that a woman recently lost her baby at the centre because the amniotic fluid was very low before she was brought to the centre.
“The pregnancy was also her first. So, by the time the baby was born, the baby was too weak and he died,”
said Mrs. Testimony.
Mrs. Testimony says she charges N5,000 for normal deliveries while she receives N8,000 for more complicated births but she takes most of the deliveries on credit which makes it easier for women to pay.
“And if the patient cannot pay, we allow them to go after 24 hours but they will make a commitment to pay. But if they don’t pay, we cannot do anything. We let them go,”
she said.
The attendant said she had no generator and had to rely on rechargeable lamps to illuminate the birth centres when there is power failure.
“I used to use my rechargeable lamp but it is now faulty. I need a generator or I will use lanterns,”
she says.
Taking the reporter around her centre, Mrs. Testimony admits that hygiene remains a problem for all traditional birth centres but they make do with what they have. She says despite these challenges, however, rural women still prefer her services.
The birth attendant explains that although government hospitals claim to be free, it is not always so. She says:
“Pregnant women in labour are asked to buy many things when going to hospital. They are also given a list of drugs to buy.”
The attendant says she has a special arrangement with some private hospitals where she refers pregnant women to when a delivery becomes complex
“At the height of the COVID-19 pandemic, I took deliveries normally and there was no problem whatsoever. I admit that some birth attendants are very careless in this job. Some pregnant women have high blood pressure. If it is not well monitored, she could go into shock during labour.
Some of them are lucky such that it is only the baby it affects and then the mother survives. Bleeding after birth also causes maternal deaths. Those of us who are good at this job, usually refer patients quickly to hospitals when such happens,”
says Mrs. Testimony.
At the centre sat Mrs. Karimat Sodiq, who is unemployed. She said she had given birth to two babies at the centre and they were fine. She, however, said in February, she gave birth to a baby at the centre and she died minutes later.
According to Mrs. Sodiq, she never did any scan throughout her nine-month pregnancy even though the WHO recommends four to eight ante-natal visits to a hospital during pregnancy.
She said health facilities were too expensive while their personnel were too impatient and obnoxious hence the decision of many pregnant women to continue to use the services of traditional birth attendants.
Mrs. Sodiq stated,
“I have given birth to three babies in this centre. Two survived but one didn’t. I really don’t know what caused her death because when the baby was born, he was OK and then she died. I think the pregnancy was high risk because I had a lot of pain for months. When the baby was born, she just started gasping for breath and then died.”
When asked if she would return to the traditional birth centre for her next delivery, she responded,
“I will come to deliver the baby at this centre because the attendant is very nice to me. I don’t like government hospitals. I just don’t like them. Even if it is free, I will not use a government hospital.”
At Oore Ofe traditional birth centre at Korukoru slum, a woman, Mrs Aminat Adeniyi, who recently lost her baby, wails over her predicament.
She, however, blames the government hospital and not the birth centre where the baby was pronounced dead.
Mrs. Adeniyi said the government hospital provided free services for pregnant women but the women usually paid for other ancillary services like ultrasound scan and drugs which were provided for by a separate facility. She said,
“I recently lost my baby. I had been going to Ade Oyo hospital for ante-natal care. I had two babies at that same hospital and I trusted them. The pregnancy was already in its 10th month. On the day I was to give birth, they said my condition was not good, that I had malaria and then they referred me to the University College Hospital. But UCH is too expensive. So, I ran down to this birth centre but by then it was too late
“During delivery, the baby’s head came out but then it got stuck. I was also losing breath already. But with a lot of prayers, we were able to get the baby out and he was already dead. I went through a lot of pains. I blame the government hospital for the loss of my baby.”
The birth attendant, Janet Obisesan, boasted that she had a 100 per cent success rate, adding that any baby that died at her centre must have been a stillbirth.
She said rural women prefer traditional birth centres because the attendants are nice and not proud like those in hospitals.
“They like us because we are nice to them. We are not like the midwives in hospitals who are educated but proud. We treat them with love and that is something that pregnant women need. I don’t have any equipment here as you can see. Sometimes, pregnant women refuse to go to hospitals unless I accompany them.
“The problem I have in this centre is the leaky roofs which cause rain to enter and wet our beds. Our toilets are not good but we have no money. My mattresses are bad but I don’t take deliveries on floors. I don’t have generator and I have to use lamps but if there is no light, I use candles,”
she says.
Damning health statistics
According to UNICEF, in Nigeria, each year, about 262,000 babies die at birth, the which is the world’s second highest national total, while every day in Nigeria, 257 babies die within their first month of life. Most of these children died from preventable causes such as premature birth, complications during delivery, and infections like sepsis and pneumonia, a violation of their basic right to survival.
“In Nigeria today, only one out of every three babies is delivered in a health centre, decreasing a newborn baby’s chance of survival.
This is just one of the issues that need to be addressed in order to improve the chances of survival of those babies born today and every day. We can save millions of babies if we invest in training and equipping local health workers so that every newborn is born into a safe pair of hands,”
says UNICEF.
UNICEF’s Every Child Alive campaign calls for immediate investment to deliver affordable, quality health care solutions for every mother and newborn.
These include a steady supply of clean water and electricity at health facilities, the presence of a skilled health attendant during birth, ample supplies and medicines to prevent and treat complications during pregnancy, delivery and birth, and empowered adolescent girls and women who can demand better quality of health services.
Over 40 per cent of stillbirths occur during labour due to hypoxia (oxygen deprivation), placental obstruction and other delivery and labour related complications. UNICEF says India, Pakistan and Nigeria have the highest rate of still births in the world, adding that still births can be avoided if key interventions, such as assisted vaginal delivery, skilled birth attendants or emergency C-sections, which traditional birth attendants cannot provide.
Stillbirth rates are higher in rural areas than in urban areas and socioeconomic status is also linked to a higher incidence of stillbirth
But the statistics is not just damning for babies. According to the Nigeria Demographic Health Survey, one Nigerian woman dies in childbirth every 10 minutes, and one Nigerian child under five years of age dies every minute.
According to the World Health Organisation, Nigeria is a country where nearly 20 per cent of all global maternal deaths happen. The United Nations also states that Nigeria accounts for 19 per cent of the world’s maternal deaths and nearly a tenth of all newborn deaths most of which are avoidable.
Experts blame TBAs
But several experts says contrary to success claims by birth attendants, their lack of skill has contributed largely to the high infant and maternal mortality. Speaking with our correspondent on the telephone, Dr. Godwin Ntadom, a Gynaecologist and Chief Consultant Epidemiologist of the Federation in the Ministry of Health, said traditional birth attendants had contributed to the high maternal and infant mortality rate in the country.
He said the government of Nigeria doesn’t recognise traditional birth attendants as health care providers and described them as a danger to the health sector. Ntadom said,
“The traditional birth attendants have no standard or educational curriculum guiding their operations because of that, they are no longer recognised as care providers. Studies also show that they do more harm than good. It is a business enterprise to them. That is where they eat from so they will never admit failure or deaths.
“What they do is that when they realise that a patient is not doing well and is about to die, they transfer patients to hospitals which often times, is too late. That is why their work is more dangerous than any other provider.
“They have a role to play since they live in the community and people know them. They can do other work but not delivery. For instance, they can remind pregnant women when to take their medicine and even lead women to hospitals but instead of doing this, they take delivery.”
When asked if the traditional birth attendants could be trained to take deliveries, Ntadom said it would be of no use because most of them do not accept training but stick to their traditional and cultural practices.
Also speaking, the First Vice President, National Association of Nigerian Nurses and Midwives, Mrs. Margret Akinsola, said traditional birth attendants have no right taking delivery of babies.
Akinsola said many of the traditional birth attendants who trained as auxiliary nurses, were only expected to assist pregnant women. She said,
“They are auxiliary health workers. Nobody should call themselves nurses because they have no training which is expected to be three years. They are adding to child and maternal health. Are they even performing well? Their so-called success stories are often exaggerated.”
Akinsola stated that most of the traditional birth centres refuse to refer patients to hospitals because they feel it makes them lose customers.
When asked to respond to allegations that rural women avoided government hospitals because of the bad attitude of the nurses, Akinsola said this was not completely true. She, however, stated that many midwives and nurses were overworked and could sometimes take out their frustrations on patients. She said,
“I will not deceive you, if you are overworked, if two patients are to be attended to by one nurse and you have 35 patients to one nurse in the labour ward, what happens when you are overworked? There is nobody who is overworked that will not react negatively.
“There is always a reaction to any action that is deleterious to one’s health. So, by the time you are overworked, there is the tendency to overreact but it is not in all cases. Like I said, a situation where you have nothing to work with, you have to tell them to go and buy items.”
Banning TBAs
A former Commissioner for Health in Ondo State, Dr. Dayo Adeyanju, who oversaw the Abiye (Safe Motherhood) programme in the state, told our correspondent that the best way to curb the infant and maternal mortality is to ban the traditional birth attendants outright.
Adeyanju, said the Abiye programme, which was commended by the World Bank for reducing the maternal and child mortality in the state by 50 per cent, was largely successful because the state government banned traditional birth attendants from operating and instead paid them to refer pregnant women to government hospitals
The former commissioner said traditional birth attendants were fond of exaggerating their abilities and hiding their failures from the public hence the absence of statistics as regards the number of babies and pregnant women that die in their centres. He said,
“When we were interacting with the birth attendants, we had about 18,000 referrals from them inclusive of 49 set of twins, 13 triplets and one quadruplet. Now, tell me how any traditional birth attendant would successfully deliver a quadruplet or triplet.
“Because the truth is that one bedroom apartment or corner of a church which is being used to take deliveries, first and foremost has no ambulance services, has no emergency preparation, has no oxygen, birth transfusion equipment and their set up is very unhygienic. So, if one baby is safely delivered and the other one is impacted, how do you manipulate and get that one out?
“What do you do if bleeding comes? So, yes, you can take delivery if it is normal. All you need to tell the woman is to push and the baby is out. But if the baby has failed to turn upside down or is facing down with its buttocks or lying in a transverse position, how do you tell her to push without rupturing the uterus? Would you be able to suture immediately and give blood? So, forget their stories. They have no success stories.”
Adeyanju said governments planning to ban traditional birth attendants must first provide alternatives from them or else the plan would fail.
The former commissioner said governments at all level must avoid the temptation of partnering with traditional birth attendants to take deliveries. He stated,
“What did we do? We bought mobile phones for about N3,000 or N4,000, bought SIM cards of N100 each and then we ensured that the phones were user free which was about N500 a month. So, N500 multiplied by seven months in order to save a woman’s life is not too much.
“The pregnant women were given the phones. And then when we started Agbebiye for the birth attendants, we started giving them mobile phones only after they agreed to be referring all their patients to us.
“Every referral costs N2, 000 and so when you refer 100, that is N200,000. Then we trained them on other vocations like baking, tie and dye. We trained then and then empowered them with a soft loan of N100, 000 each to set up a business.”
Speaking with this newspaper, however, Abiodun Adereni, who runs an NGO, Helpmum, committed to providing essential tools for delivery in rural areas, said traditional birth centres are filling a gap and must thus be encouraged by the government rather than hounded.
Adereni, who has begun renovating some of the birth centres, further stated that shutting down traditional birth centres would be counterproductive since most of the health facilities were far from rural communities.
“Even if the government builds hospitals in every community today, the women will still opt for TBAs. There is a need for a campaign for behavioural change first.
Let the government partner with TBAs and help them renovate their centres like what we are doing. Let the government attach doctors to some of these TBAs and you will witness a massive drop in maternal and infant mortality cases,”
he said.



